You are currently browsing the tag archive for the ‘IUI’ tag.
WEEK OF FEBRUARY 9, 2009
It is so interesting…we got home and said, Okay, let’s take the week to determine what to do, IVF or IUI. But I think we both knew right away that IVF was the way to go. Like I said, I tend to get all the info and have the ability to make a decision immediately. The hubby? He ruminates. I get it. And then I don’t get it. At the same time, it did feel a little strange to meet one time with a doctor and then make a major life altering decision. We decided to do the following:
- Talk it over with our parents
- Review the financial ramifications of trying IUI first, then moving on to IVF if IUI was unsuccessful.
- Complete a list of unanswered questions to email to Dr. F.
IUI
To begin, we learned more about the IUI process. Most people we know call it “The Turkey Baster.” I guess this is the way they can make is comfortable to talk about. {Maybe this is something I’ll talk about later, how much people DON’T want to talk about this, even your closest friends.}
IUI is defined as the process by which sperm is deposited in a woman’s uterus through artificial means. From what I have read, many IUI candidates are those who have male fertility issues and can use assistance getting the “good” sperm separated and inserted past the cervical mucous.
Process
TheAdvanced Fertility Center of Chicago has a good description of the process in my opinion:
- The woman usually is stimulated with medication to stimulate multiple egg development and the insemination is timed to coincide with ovulation – release of the eggs from the follicles.
- A semen specimen is either produced at home or in the office by masturbation after 2-5 days of abstinence from ejaculation.
- The semen is “washed” in the laboratory (called sperm processing or sperm washing). By this process, the sperm is separated from the other components of the semen and concentrated in a much smaller volume. Various media and techniques can be used to perform the washing and separation, depending on the specifics of the individual case and preferences of the fertility doctor and laboratory. The sperm processing takes about 20-60 minutes, depending on the technique utilized.
- A speculum is placed in the vagina and the cervical area is gently cleaned.
- Then the separated and washed specimen consisting of a purified fraction of highly motile sperm is placed either in the cervix (intracervical insemination, ICI) or higher in to the uterine cavity (intrauterine insemination, IUI) using a sterile, thin and soft catheter. Intrauterine insemination has a better success rate than intracervical insemination. Therefore, it is the preferred method at the large majority of fertility specialist centers.
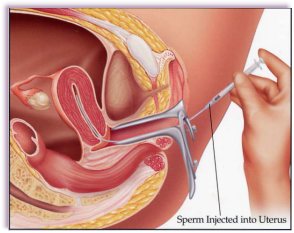
IUI Insertion Example
After reviewing this option, my husband is REALLY, REALLY wanting to do this. He feels like it is more natural, in so much as those procedures that need assistance. He is getting pretty upset that our baby may be made in a petrie dish. I keep joking we can name the baby Pete. Apparently, not so funny. I think it is. The other consideration here, this is MUCH LESS invasive and emotionally and physically demanding on the woman. My husband did not want to see me go through this.
IVF
I thought I knew a lot about this process. You take some hormones, they harvest your eggs, they fertilize them, re-implant them and you are pregnant. Yippee! I DID NOT KNOW. I JUST DID NOT KNOW. Every situation is quite personalized For us, we were starting from a poor baseline. Let me take you through the process of IVF, later I’ll talk about follicles, eggs, etc.
IVF has many steps, and is much more complicated to explain than IUI. In short, the goal of IVF is to stimulate more than multiple follicles {as opposed to one} into multiple eggs for retrieval and fertilization in a lab. These fertilized embryos will be implanted into the woman’s uterus anytime between 2-5 days after fertilization. Two weeks after implantation you will know if you are pregnant. I will go into MUCH greater detail the IVF process in a later post.
TALKING TO OUR PARENTS
This just didn’t go so well. My hubbo isn’t that close to his, so we went to talk to mine. I just started to cry. I startled myself with this. They just didn’t think it was as “bad off” as we said. My dad, the doctor, was convinced that our test results were wrong. Bless them, they just didn’t want to see us in pain.
OUR LIST OF QUESTIONS
- You quoted us possible success rate of 35-40% with IVF. Is this per embryo implantation per cycle, or per cycle only? And, is this rate based on our specific case?
- How many eggs will you aim to retrieve? What is a normal retrieval?
- How many eggs do you recommend implanting per cycle?
- What is the increased percentage of multiple births?
- What is the risk for miscarriage?
- What are the common complications we need be aware of?
- Is it possible that our future bloodwork and/or tests could change our eligibility for IVF treatments? Are there key tests we need to be aware of?
- Are there any genetic defects and/or development disorders that have been associated with / attributed to IVF?
- Given our inclination to move straight to IVF, do I need the laparoscopy, or can we wait?
- I have recently gained about 15 pounds (normal weight is 160-165lbs). Is there benefit to waiting a couple of months to lose the weight prior to starting treatment? I am concerned about being too heavy during my pregnancy.
- Is there weight gain associated with the fertility drugs I will be taking?
- Are there any lifestyle modifications that might help my condition and increase my chances of getting pregnant? What role do the following play in getting pregnant: weight, exercise, prescription drugs, stress, acupuncture, etc?
- What is the full array of programs/services the Center for Reproductive Health offers?
- Will any of our fertility conditions worsen over time, improve, or remain constant?
- What further tests do you recommend? Are there any risks associated with the testing? Does my hubby need additional testing?
- Follow up: In your practice, how often does this/these treatment(s) result in pregnancy? How many of these pregnancies result in live births, miscarriages, etc. (percentages?)
- How many cycles of treatment on average does it take to see positive results?
- Can we begin treatment immediately? Do you tailor treatment to individual couples, or is there a set protocol?
- What type of monitoring and interaction can I expect from the center? Ultrasounds, blood work, general communication? How available are people for consultation and questions via telephone?
- What are the benefits to IUI v. IVF? What makes a good candidate for each treatment? Can we improve our candidacy for IUI?
- At what point do either or both of us need to consult a reproductive endocrinologist? Does your center offer that service?
- Do you provide fertility and ob/gyn, or fertility only? Do I need separate ob/gyn?
- What does treatment cost? Does my insurance cover any of the medications, hospital charges, or doctor’s visits? If I must pay out-of-pocket, do you offer any special payment plans?
- What is the procedure for getting questions answered between appointments? Can I call, fax, or e-mail and expect a prompt reply?
- What is the standard callback time, and does it vary depending on the urgency of the call?
- I understand that many of my questions can be answered with a callback from a nurse, but if I need to speak with a doctor how do I make that clear?
- What do I need to know about scheduling weekend procedures?
- What is the phone number for off-hours problems?
- Is there a directory of phone numbers for office staff and doctors? (numbers for contacting a nurse, getting lab results, discussing billing issues, etc)
THE DECISION
By default, we decided to just go to the upcoming IVF orientation. We were pretty clear that IUI was not going to work for us. Had it simply been an issue of my husband’s sperm motility, it may have made sense. However, with my follicle count and FSH levels “drifting upward” we knew we needed additional help. At this point, I think it was really more a question of whether or not IVF would work for us.
MONDAY, FEBRUARY 9, 2009
Today is the day. We have our big appointment with Dr. Victor Fujimoto at the UCSF Center for Reproductive Health. I have been counting down the days. Like Christmas. Remember when you were little, and it seemed like time stretched on and on and on? Then you get to the day and you wonder, what is in store for you?
I had been preparing for weeks. I wanted to know as much as I could as to speak intelligently to the doctor. I didn’t know if he would be the God Complex type or the compassionate type. Would we have much time with him? Or would this just be a quick meet and greet and then he would send us off for more testing. Having most of the preliminary testing done beforehand was a good idea, I thought. {In the end, Dr. Fujimoto was pleased with that as well.}
My husband has a completely different approach. He prefers to hear what the doctor says, then ask questions based on results. This does make me a bit nutty. I think we should have questions prepared for all the options. We STRONGLY disagree here. What a learning lesson for me. I have to remember that we don’t have to think alike, or be the same. And I can’t expect him to act and think like I do. You know, it is probably better that we are different that way…he may be more open to hearing things I don’t since I have everything written down. I tend to get stuck in what I have in my mind.
We arrived for our appointment a few minutes early. I was happy my husband was ready on time, and we were there with time to spare. My husband likes to breeze in at the last moment, rarely thinking of the details that need to be taken care of when we arrive places-is there paper work to fill out…do we need to bring a gift or wine to a dinner party…will we be checking bags at the airport? This is how we ultimately compliment each other.
The women at the front desk were so kind, and knew us both by name. This made me feel so easy, like we were not just another name in their book. The offices were very nice, and well kept. When we walked in, and I was filling out the paperwork, I noticed my husband seemed a bit distant, glassy-eyed. I think the full weight of what was happening hit him at that moment. We had talked a lot about it, but you can never really prepare until you are in a situation, I think. And, he has so much going on at work right now, I know he hasn’t really had the bandwidth to process all of this. He has told me time and again how much he has wanted a “natural baby.” He wants a family so badly, he will do what it takes. And, we will adopt if we can’t have out own. But I know that the idea of the petrie dish makes him sad. Being the romantic that he is, the clinical nature of this knocks the wind out of him.
The nurse called me in to do my initial vitals…weight, blood pressure, temp…and I wonder, why do I wear boots, jeans and a heavy sweater? My weight shows a solid 5-7lbs more than normal. What a chub. I have gained about 15lbs since our wedding. Most people like to say, oh, married life. Really, I have just felt so ill this year that I have not made it to the gym much lately. I promised myself in that moment I would do what I could to drop some weight before we began a cycle. It would be at least 8 weeks. I can do some serious damage in that time! It really just takes focus on my part, and discipline on my husband’s part. He doesn’t like to eat his ice cream alone, so I really have to get him to promise not to tempt me.
Dr. Fujimoto came out to invite us to his office. I love when the doctor comes himself to the waiting room for you. They just seem more accessible to me that way. We went directly to his office, where Dr. Fujimoto had our file, preliminary testing and initial intake form. Prior to our visit, we were required to review and complete a LENGTHY packet of information. Dr. Fujimoto had clearly reviewed our packet, studied our test results and was well-prepared to meet with us. We came prepared with a list of questions and a calendar charting my menstrual cycle, LH surge, estimated ovulation and intercourse dates.
We spent about 15 minutes discussing our previous results with Dr. Fujimoto. At this point, he suggested we move into the ultrasound room where he would perform a vaginal ultrasound. Again, my husband would be with me, with a man I did not know prowling around my coochie! My husband is actually very cool about it, I am the one who is mortified. I am hoping the more we do it, the better I will feel.
Off we went, and I undressed from the waist down. At least this time the table had some cushion, was on an incline and had stirrups. HOWEVER, there was NO MODESTY with Dr. Fujimoto. I had the paper drape over my lap, and when I lay down on the table, he essentially threw it up over my waist. ohhhkaay! This was also the first time that I had a vaginal utlrasound where I did not insert the probe myself. He was not rough or anything, I was just a bit startled…my first meeting with a male doctor I didn’t know, and he was probing me! Like I said, I think it will get easier. And I think I will HAVE to get over it by the time we go in to birth the baby. I have heard that you just CANNOT care at that moment.
During the ultrasound there was a female nurse in the room (who did not introduce herself to me, huh?). Suddenly, Dr. Fujimoto became quite serious and very professional. The casual and friendly atmosphere redirected and my husband and I became silent. I was worried. And, to be honest, I was terribly sad. Heavy news was to come. Dr. Fujimoto began dictating notes to the nurse, describing the number of antral follicles found in each ovary. He gently removed the probe, asked me to get dressed, and invited us back to his office.
When we sat down with Dr. Fujimoto for our second discussion, the air in the room felt a bit dark to me. My husband and I were holding hands, we were determined to be optimistic. This was our first fertility visit, and had the idea that we would be sent for tests and take a few steps at a time towards a diagnosis and getting pregnant. We were so wrong.
For better or worse, Dr. Fujimoto was extremely candid with us. It was hard to hear, we were stunned. BUT, to say we were appreciative is an understatement. His ability to understand complex issues and explain them to people outside the medical profession is unmistakable.
Dr. Fujimoto’s assessment was:
- My FSH level, at 9.8 units/liter, was high, and drifting upward. This was a surprise as my ob/gyn had reported all my blood work to be in the normal range. Normal range is actually 4-7 units/liter.
- I had a significantly low antral follicle count of 8 follicles. A normal follicle count would be 40-50.
- My husband has a borderline low sperm count at 20million.
What did all this mean? Could we proceed with IUI? This was the recommendation from our ob/gyn. This was also the preference of my husband, it seemed the most natural option.
No. With a drifting FSH level, my ovaries and egg quantity are likely compromised. I have a low ovarian reserve, and, like most women, am shedding close to 1,000 follicles per month. IUI would provide us less than a 10% chance per month of conception. IVF would provide us a 35-40% chance per month of conception. Dr. Fujimoto strongly recommended us to move straight to IVF. Indeed, he said that if we wanted to have a family, this was our time. In fact, we had no time to waste.
We left with a handful of cards for the IVF team…the coordinator, the nurse, the billing team, the urologist…I’m sure there are more I can’t remember right now. We all agreed we would spend the weekend deciding what to do and contact Dr. Fujimoto the following week with a decision and/or any follow up questions.
My husband and I walked into the elevator holding hands in complete silence. It is not like me to not start chatting right away. I like to know what he is thinking. I usually need to pry it out of him. I was in shock, though, that we had to move to the most drastic fertility procedure from the get-go. As we walked outside, my husband ran his hands through my hair, rubbed the back of my neck, and kissed the bridge of my nose. I always know how much he loves me when he does this. I couldn’t have married a better man.
I had my annual exam October 2008. At this time, I pressed the issue with my ob/gyn regarding next steps aiding our fertility. I was disappointed by her knowledge, or lack thereof, of both male and female fertility issues. This doctor is one of the most reputed in Northern California, and has been mine since I was 17 years old. When I asked her a few (in my opinion) basic questions, she was unable to answer them to my satisfaction. In general, I found her answers vague, uninformed and lacksidasical.
A few of the questions I asked:
- Is there any concerns that my previous inclination toward cyst development is impeding my ability to get pregnant?
- Has the amount of / duration of time I have taken birth control pills affected my ability to ovulate, and thus get pregnant?
- What do you make of my cycle length(s)? (They were erratic for the first 4 months, then regulated at 24/25 days)
- Are there dietary or environmental changes I can make to affect potential conception?
At the end of the exam, based on my short cycle length, my doctor recommended we begin a course of Clomid treatment for 3-6 months. Should this be ineffective, she recommended we see a specialist. She briefly explained to me that Clomid is the most common first-line fertility treatment used, roughly in about 25% of women with trouble conceiving. The purpose of Clomid is to establish a regular ovulation pattern. Unlike many other fertility medications which promote the production of more eggs from follicles, Clomid focuses on regular development of a single egg.
I left my appointment a bit frustrated by my doctor’s lack of knowledge, but excited to have a direction. I was off to my computer to do a little research. Google can be both a blessing and a curse in these situations.
MY ADVICE: Always proceed with caution! There is a TON of information out there, and at a certain point, you have to shut it all out and have a direct conversation with your provider to understand the best course of action for your case.
None the less…after a bit of research, my husband and I concluded that there were several tests that were supposed to be ordered prior to Clomid therapy. Additionally, I was suspect as to whether or not Clomid was the right course. After several messages to my doctor’s office, I was able to speak with her. She ordered the following tests:
- Day 3 FSH levels
- Day 7 LH and Thyroid
I went into the office the following day to pick up the blood work order. Attached to it was a form checklist / cover page with the title “Infertility Testing”. {I HAVE TO SAY: I actually paused, albeit the briefest of moments, when I read that walking down the hallway. It hit me that after all these years of dreaming of my perfect husband and beautiful children, all the years of loving my nephews unconditionally, all the years of gushing over my friends’ children, I was the one who was going to have trouble having a baby. All the late nights I had worked, the fantastic trips I had taken, the unbelievable experiences I had slipped away in one breath knowing I may have waited too long.}
This checklist included the description of 6 different tests the doctor may run to determine initial fertility issues. I wondered why we hadn’t discussed this previously? I read all of them, and their descriptions, noted the ones with “X” by them indicated I needed to complete, and then studied the others crossed off-as though I wouldn’t need to worry myself with those. Oddly, I did. I read them, and googled them to get an idea of the trajectory of testing ahead.
THE CHECKLIST
- Day 3 FSH (Follicle Stimulating Hormone) blood test
- Day 7-10 LH (Luteinizing Hormone) blood test
- Hysterosalpingogram (HSG)
- Hysteroscopy
- Exploratory Laproscopy
- Semen Analysis (PHEW! One that wasn’t for me!)
When I asked about the other tests, I was told that I would likely not need any of them. When I talked to my husband, mother and father about them, they told me I was being dramatic, and not to get ahead of myself. I just felt something was off.
At this time, I was VERY adamant with my husband that he get the semen analysis order from his doctor. I wanted to know on both sides what we were dealing with.
So, we were off! Testing was under way. We continued to have sex, during the right and “wrong” times 🙂 We used the mucous test and the First Response Ovulation Predictor Kits to determine my ovulation. When it was time, we had sex every other day. Based on my husband’s age (42) we were told he needed a day to regenerate good sperm.
